|
Cataract
Cataracts
Cataracts
Your eye works a lot like a camera. Light rays focus through your lens onto the retina, a layer of light-sensitive cells at the back of the eye. Similar to photographic film, the retina allows the image to be “seen” by the brain.
Over time, the lens of our eye can become cloudy, preventing light rays from passing clearly through the lens. The loss of transparency may be so mild that vision is barely affected, or it can be so severe that no shapes or movements are seen—only light and dark. When the lens becomes cloudy enough to obstruct vision to any significant degree, it is called a cataract. Eyeglasses or contact lenses can usually correct slight refractive errors caused by early cataracts, but they cannot sharpen your vision if a severe cataract is present.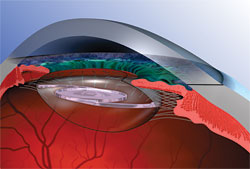
The most common cause of cataract is aging. Other causes include trauma, medications such as steroids, systemic diseases such as diabetes, and prolonged exposure to ultraviolet light. Occasionally, babies are born with a cataract.
Cataracts typically develop slowly and progressively, causing a gradual and painless decrease in vision. Other changes you might experience include blurry vision; glare, particularly at night; frequent changes in your eyeglass prescription; a decrease in color intensity; a yellowing of images; and in rare cases, double vision.
As the eye’s natural lens gets harder, farsighted (presbyopic) people, who have difficulty focusing up close, can experience improved near vision and become less dependent on reading glasses. However, nearsighted (myopic) people become more nearsighted, causing a worsening in their distance vision. Some kinds of cataracts affect distance vision more than reading vision. Others affect reading vision more than distance vision.
Reducing your exposure to ultraviolet light by wearing a wide-brimmed hat and sunglasses may reduce your risk for developing a cataract, but once one has developed, there is no cure except to have the cataract surgically removed.
With a routine, outpatient surgical procedure, an ophthalmologist (Eye M.D.) can remove the cataract, making either a small incision 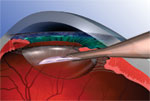 (phacoemulsification) or a larger incision (extracapsular extraction). Usually, a synthetic intraocular lens (IOL) is inserted at the time of cataract extraction to replace the focusing power of the natural lens. IOLs can be monovision (fixed-focus for a preset distance) or multifocal, which allows focused vision at many distances. The time to have cataract surgery is when the cataract is affecting your vision enough to interfere with your normal lifestyle.
(phacoemulsification) or a larger incision (extracapsular extraction). Usually, a synthetic intraocular lens (IOL) is inserted at the time of cataract extraction to replace the focusing power of the natural lens. IOLs can be monovision (fixed-focus for a preset distance) or multifocal, which allows focused vision at many distances. The time to have cataract surgery is when the cataract is affecting your vision enough to interfere with your normal lifestyle.
Cataract surgery is a very successful operation. One and a half million people have this procedure every year in the United States, and 95% have a successful result. As with any surgical procedure, complications can occur during or after surgery, and some are severe enough to limit vision. But in most cases, vision, as well as quality of life, improves.
Questions Frequently Asked By Patients:
Why Outpatient surgery?
Medical knowledge has advanced to such a degree that now outpatient surgery can be performed for many surgical procedures. Cataract surgery is one of these procedures. It allows you to resume your normal activities almost immediately. Our experience is that patients enjoy returning home after the surgery to eat thier own meals, take their own medications, and sleep in their own beds. Some patients even go shopping on the way home or play cards that afternoon.
Will I be awake during the operations?
Yes, you will be awake during the operation, but you will be given light sedation that will help you to be very relaxed and calm.
When can I drive?
Driving is not permitted until after your first post-op visit to our office. The doctor will determine if driving is permitted based on your vision. If you have questions about driving, please discuss this with the doctor.
When may I wash my hair?
You may wash or brush your hair any time after the surgery.
May I wear my own glasses?
You may wear your glasses. The lens in the glasses over the eye that had surgery will not be very useful to you. We will be changing that lens in your glasses after the eye recovers from surgery.
When do I get my new glasses?
It takes approximately 3-5 weeks for total healing to take place. The final glasses presription will be determined at that time.
May I travel?
Yes, you may travel right after the operation.
How many post-op visits will I need?
This is the usual procedure: the first visit is the next day after surgery; the second visit is 3-4 weeks later.
when can I resume my activities?
You may resume your normal activities right away with very little deviation from your regular life-style.
How long should I wear my eye sheild?
The eye shield is solely for protection to prevent you from accidentally rubbing or injuring the eye. Wear it during sleeping hours for one week.
The Surgical Experience
In the pre-op area you will be given several eye medications. These drops dilate your pupil, help prevent infection, as well as numb the surface of your eye.
A small IV catheter will be placed in your hand or arm so medication may be given to help you feel very calm and relaxed. In some instances, an anesthetist may give you medicaiton in the IV that will make you sleepy for a few minutes. During this time, a local anesthetic will be given. When you wake up your eye will be numb and you will be relaxed and calm.
The Operation
When you arrive in surgery, the nurses will see to your safety and comfort. You will have an EKG monitor and blood pressure cuff on. Your face will be covered with a sterile plastic sheet, but you will be able to breathe normally because you will receive oxygen under the sheet.
Immediately After Surgery
You will be taken back to the post-op area and given a light snack. The nurses will monitor your prosgress and allow you to go home when they are satisfied that you are alert and awake. You will receive post-op instrutions.
Same day at home
Resume your normal activies. Resume any medication you were taking from other doctors as ordered when you get home. Your eye may feel scratchy and itchy. you may take Tylenol as needed for any eye discomfort or irriation. Keeping your eye closed will help you feel more comfortable. DO NOT RUB THE EYE. If your eye tears, close it gently and wipe the tear away as it reaches your cheek. Do not put any pressure on the eye. Your vision will be blurry the first day because the pupil is dilated.
Instructions for Surgical Patients
Medications
If you normally take heart, blood pressure or breathing medications in the AM. You may still take them with a sip of water. Diabetics on insulin and pills: do not eat anything after midnight the night before surgery. You may drink 4 ounces of water up to 2 hours before your arrival time. Bring your insulin or pills withyou on the morning of surgery.
Food
Do not eat anything after midnight before surgery. You may drink 4 ounces of water up to 2 hours before your arrival time.
Bathing
A bath or shower should be taken the evening before or the morning of surgery. On the morning of surgery wash face thoroughly and DO NOT apply moisturizer or make up. Men should shave. You may brush your teeth.
Dentures, Glasses, Hearing Aides, Etc.
It is O.K. to wear dentures and hearing aides. You will need to remove your glasses during surgery.
Clothing
Wear loose comfortable clothing. Please wear a short sleeve shirt/blouse. We will give you a gown to wear. You will keep your slacks on.
Transportation/Reponsible Party
You will need someone, other than yourself, to drive you to and from the office the day of surgery and to your post-op visit the next day. On the day of the surgery, you will need to have a responsible adult with you to receive post-op instructions and accompany you home.
Visitors
Please restrict family and friends in the waiting room 1 or 2 people.
Locker with Key
A locker with key is available for your valuables, or they may be left with a family member or friend who accompaines you. We cannot take responsibility for personal items such as rings, watches, bracelets, etc.
How to care for your eyes after Cataract Surgery
After your surgery is completed, it will be important for you to know how to care for your eye properly. This information will guide you in your eye care.
The day after
The day after surgery, your eye will begin a time of healing. You will notice changes in your vision during that time and you can expect your sight to get better as your eye heals.
Time to heal
You eye will need three to five weeks to heal properly. During this healing period, we may examine your eye several times to monitor your progress. In the first two weeks after surgery, you may experiance some common and normal irritaions. They are:
- Redness of the eye
- Scratchiness in the eye
- Watering eye
- Discharge or crusting on the eyelids, especially in the morning
- Specks or threads in your vision
- eye will be sensitive to light; tearing may result from sunlight (wear sunglasses as needed)
- tenderness around the eye; you may take mild pain relievers (Tylenol) as neeeded.
Typically, all these signs will improve as the healing time continues.
Warning sings which require our immediate attention are: Please Call the office at 810-238-3603
- Severe, prolonged, unrelenting pain or discomfort in and around the eye.
- Sudden change in vision.
- Bright burst of light followed by reduced vision.
General Eye Care
Wash discharge from eye with clean wet face cloth for one week, if necessary.
What will I be able to do?
You will be able to engage in most activities. You may be up and about, bend over to pick up objects or put on shoes. Using reasonable care, you may bathe or shower, wash hair, shave, brush teeth, read, write, watch TV, ride in care, climb stairs or go for a walk. Driving is permitted, following your first post-op visit, if the other eye sees well enough. You may sleep in any position you desire. You may lie on either side.
Eye protection
It is important not to rub the eye that was operated on. It is always important to protect the eye from unexpected injury. Use the eye sheild while sleeping for one week following the surgery. Run the tape (which holds the shield in place) from the center of your forehead down toward the lower part of the ear. If you have any pain or unusual symptoms, please call 810-238-3603. If the office is closed please leave a message with the answering service and someone will return your call.
Instructions for use of eye medications
Drops should be placed in the space between your eye and lower lid as follows:
- Wash hands thoroughly before touching the eye area.
- Placing a finger on your check, just under your eye, gently pull down until a "V" is formed creating a pocket between your lower lid and eye.
- Being careful not to touch the tip of the eye drop container with your fingers, or to the eye, instill drops as ordered.
- Continue to hold the lower lid out for a few seconds.
- Release lid.
- Close eye slowly. DO NOT SQUEEZE EYE!
- Wipe away excess medication with clean tissue or gauze.
Multifocal Lenses to Treat Cataracts
When you have a cataract, the lens of your eye becomes cloudy. Light cannot pass through the lens easily, and your vision becomes blurred. During cataract surgery, the ophthalmologist (Eye M.D.) removes the cloudy, natural lens and replaces it with a clear, artificial lens called an intraocular lens (IOL). The IOL helps your eye regain its focusing ability and allows you to see clearly again.
The most common type of IOL is the monofocal or fixed-focus IOL. The monofocal lens helps you attain clearer vision at one distance. Note that eyeglasses and contact lenses are still required in order for you to see clearly at all ranges of distance.
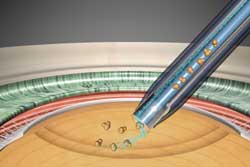
Another type of IOL is the multifocal IOL. The multifocal lens has several rings of different powers built into the lens. The part of the ring you look through will determine if you can see clearly at far, near, or intermediate distances.
Implanting an IOL takes about 20 minutes and is an outpatient procedure. In addition to a preoperative eye exam, your eye surgeon will take some measurements of your eyes and will give you topical or local anesthesia. The surgeon makes a few small incisions close to the edge of the cornea and then inserts a small, ultrasound instrument to break up the center of the eye’s natural lens. The lens is then vacuumed out through one of the incisions. The surgeon folds and inserts the IOL through the same incision. These incisions are usually self-sealing, requiring no stitches. Once implanted, a multifocal or accommodative IOL allows you to focus on near or distant objects.
Risks associated with implanting IOLs include overcorrection or under-correction, infection, increased floaters, retinal detachment, dislocation of the implant, halos, glare, dry eye, decreased contrast sensitivity, clouding of a portion of the IOL, and loss of vision.
If you are going to have cataract surgery, you and your ophthalmologist should discuss which IOL may be best for your vision needs.
Phacoemulsification
 Phacoemulsification (Phaco) is a surgical method used to remove a cataract, which is a clouding of the eye’s naturally clear lens. A cloudy lens interferes with light passing through to the retina, the light-sensing layer of cells at the back of the eye. Having a cataract can be compared to looking at the world through a foggy window.
Phacoemulsification (Phaco) is a surgical method used to remove a cataract, which is a clouding of the eye’s naturally clear lens. A cloudy lens interferes with light passing through to the retina, the light-sensing layer of cells at the back of the eye. Having a cataract can be compared to looking at the world through a foggy window.
In phacoemulsification, an ultrasonic oscillating probe is inserted into the eye. The probe breaks up the center of the lens. The fragments are suctioned from the eye at the same time. A small incision that often does not require sutures to close can be used, since the cataract is removed in tiny pieces. Most of the lens capsule is left behind and a foldable intraocular lens (IOL) is implanted permanently inside to help focus light onto the retina. Vision returns quickly and one can resume normal activities within a short period of time.
Posterior Capsulotomy
A posterior capsulotomy is a laser procedure that sometimes is necessary after cataract surgery.
During cataract surgery, part of the front (anterior) capsule of the eye’s natural lens is removed to gain access to and remove the lens. The clear, back (posterior) capsule remains intact and supports an intraocular lens (IOL),  a plastic or silicone disc that is implanted in the eye and replaces the natural lens. As long as that capsule stays clear, you will experience good vision. But in 10% to 30% of cases, the posterior capsule loses its clarity. When this happens, the ophthalmologist (Eye M.D.) can create an opening in the capsule using a laser in order to restore normal vision. This procedure is called a posterior capsulotomy.
a plastic or silicone disc that is implanted in the eye and replaces the natural lens. As long as that capsule stays clear, you will experience good vision. But in 10% to 30% of cases, the posterior capsule loses its clarity. When this happens, the ophthalmologist (Eye M.D.) can create an opening in the capsule using a laser in order to restore normal vision. This procedure is called a posterior capsulotomy.
Before the laser procedure, the ophthalmologist does a thorough ophthalmic examination to make sure there is no other reason for vision loss.
The posterior capsulotomy is painless and takes approximately five minutes. Eye pressure is measured 30 minutes after the operation to make sure it is not elevated, and anti-inflammatory medicated eyedrops are usually prescribed for three days following the procedure. Vision usually improves within hours.
Potential but rare complications following laser posterior capsulotomy are increased intraocular pressure and retinal detachment.
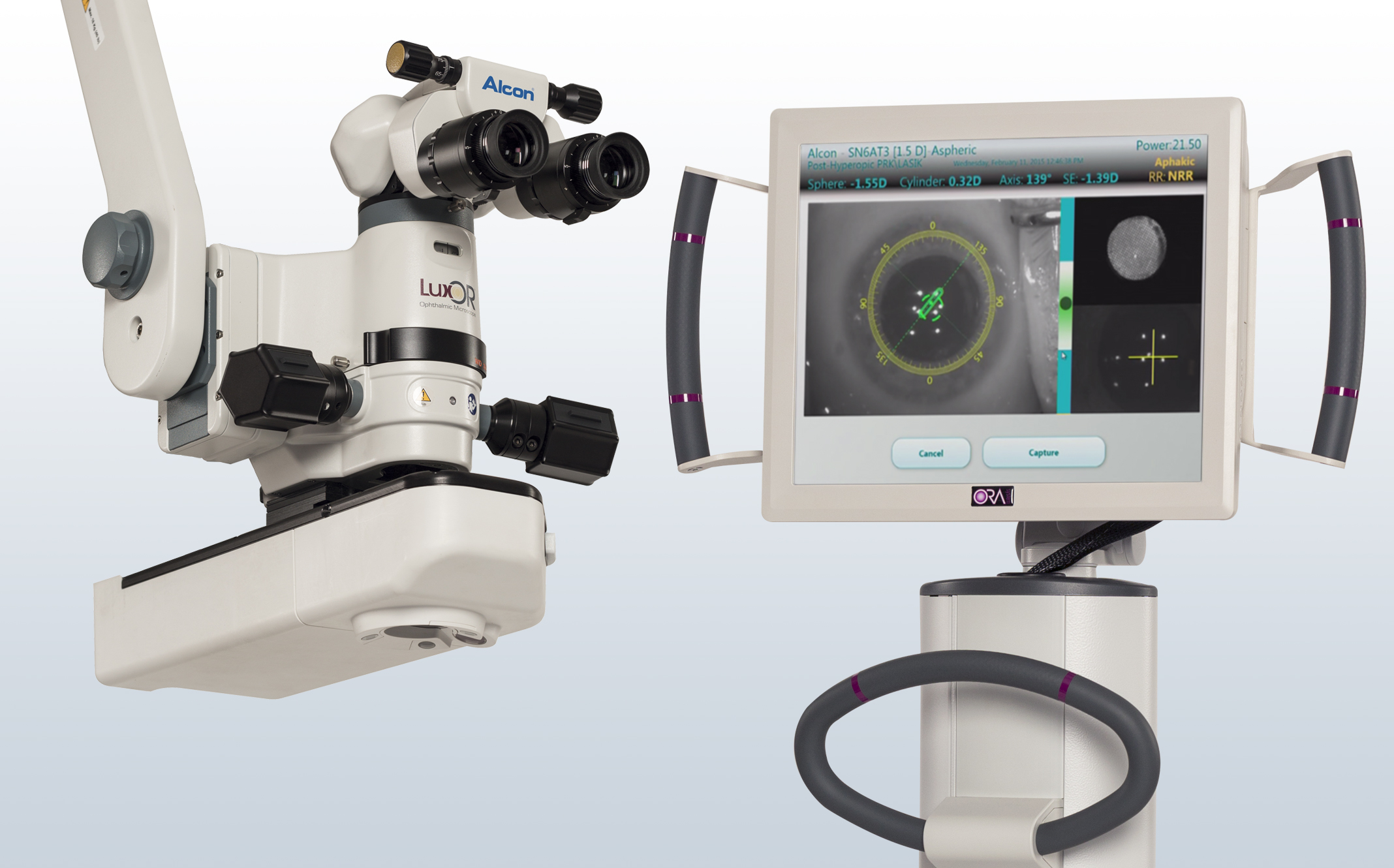
ORA System with VerifEye
ORA system with Verify is offered at the East Michigan Surgery Center as a specialized surgical confirmation tool which helps customize your vision even further during all custom cataract surgery procedures performed. The ORA ( Optiwave Refractive Analysis) intraoperative aberrometry system provides real- time analysis of your eye during surgery. During standard cataract surgery, without ORA, various measurements are taken prior to cataract surgery in order to to select the IOL or intraocular lens power but there can be a margin of error when making the proper selection based on unknown surgical factors. With the use of ORA with Verify during your cataract surgery, we can ensure your procedure will be optimized and the analysis will provide our surgeon with information that helps confirm the proper correction for optimal visual outcomes. For patients with astigmatism, those who have had prior LASIK or PRK, or those who are having a multifocal lens implanted, ORA with VerifEye can improve the accuracy to help reduce the need for glasses after your procedure.

|
Home
|
Patient Portal
|
What Can I Expect At My Appointment?
|
About Us
|
Optical
|
Patient Resources
|

|